By Dr. Korin Hudson
With the start of the school year upon us, many of us (and many of our children) are gearing up for back-to-school and fall sports. As many of our kids suit up for football, soccer, hockey and other sports, many parents worry about the risk of concussion. There have been a number of media stories lately about concussions and the long-term risk of chronic complications of injuries sustained in amateur and professional sports. But what does this mean for our kids as they lace up their cleats this fall?
What is a concussion?
A concussion is an injury to the brain that results in a temporary loss of normal brain function, usually following a direct blow or a jostling of the head. Loss of consciousness or “blacking out” is not required, and in fact- most patients do not report losing consciousness when they sustain their injury. Its best to think of a concussion as a functional injury to brain rather than a structural injury. Unlike other structural brain injuries which cause bleeding, bruising, or swelling which can be seen on CT scans or MRI, concussions affect brain function, which means that even with a normal scan patients may have significant symptoms.
Concussion symptoms may vary from patient to patient and injury to injury. Some patient’s report symptoms that start immediately after the impact, while others don’t develop symptoms until later that day, or even the following day. Symptoms usually fall into several categories: headache, neck pain, vision symptoms, balance symptoms and dizziness, sleep dysfunction, cognitive and memory deficits, and mood changes. Patients may suffer any or all of these, and they may improve at different rates.
Initial Evaluation:
If you or your child sustains and injury and you think they might have a concussion, the most important thing is to remove them from practice or competition immediately. If there is an athletic trainer or team physician on site they can do an evaluation for concussion and make a decision about the next step. No athlete should be allowed to return to practice or competition without a thorough evaluation by a healthcare professional who is comfortable evaluating athletes with concussions.
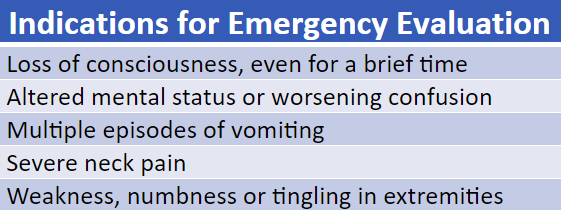
Under some circumstances, athletes should be seen in the Emergency Department at the time of their injury (see Figure 1). Athletes with any of these symptoms require an urgent evaluation by a physician and may need imaging to rule out more serious injury.
Figure 1
Treatment:
Athletes should rest for the first 24-48 hours. This may mean staying home from school and should certainly include avoiding television, computers, smartphones, and tablets. Acetaminophen (brand name Tylenol) may be taken according to package instructions. If you or your child is prescribed any medication by your primary doctor or the ER, always check before using any over-the-counter medications at the same time as the prescription medication. A follow-up appointment with your primary doctor or a sports medicine/concussion specialist should be scheduled as soon as possible to develop a plan for return to school and return to activity.
For years, injured athletes were told to stay in a dark room and do nothing until their symptoms resolve. But in recent years we have realized that most student athletes are better served by an “active recovery”. In many cases, athletes can return to school with partial days, limited note-taking, and no homework or tests during their acute recovery period. Getting back to school on even a limited basis helps the student athlete “ease” back into regular activity. During this time, audio books, short periods of reading and writing, and continued limitation on screen time may help limit symptoms. For prolonged symptoms, formal school accommodations (such as a 504 plan or an IEP) may be required, but in most cases, temporary accommodations will suffice while symptoms resolve.
In recent years we have also realized that moderate physical activity can help student athletes with concussion. Moderate exercise, such as a brisk walk, light stationary biking, etc. can in fact help reduce symptoms and can actually get injured patients back to school/work faster and back to sports sooner than athletes who do no activity at all. That said, any exercise plan should be guided by a physician, athletic trainer or physical therapist. Any light exercise should be limited to activities which do not exacerbate symptoms, and no vigorous activity (sprinting, plyometric exercises, weightlifting) or contact sports should be permitted during the acute recovery period.
Some patients will respond well to relative rest and a gradual return to exercise, but others will have protracted symptoms that may require additional treatments. Though there is not a lot of high-quality research regarding the use of medications and specific therapies for concussions, many concussion specialists do feel that medications to prevent headaches are appropriate for some patients. Some patients will also respond well to physical therapy, occupational therapy, and/or speech language therapy. Each of these therapies focuses on a different aspect of the concussion syndrome including the neck pain, dizziness and balance problems, as well as the vision symptoms and cognitive deficits.
Often, physicians are asked “how long will these symptoms last?” and the simple answer is: every patient and every concussion is different. Most athletes with a first-time concussion, who doesn’t have pre-existing neurologic conditions (such as migraines, vertigo, or seizure disorder) will be symptom-free within a month. However, patients who have had multiple prior concussions or with other medical conditions may tend towards longer recoveries. Each concussion much be approached individually.
Once symptom-free, athletes who wish to return to sports participation should go through a monitored, step-by-step return to play program. The return-to-sport guidelines have been endorsed by international concussion experts, but may need to be modified for different sports and for different athletes. Many physicians and athletic trainers will couple the return-to-play protocol with repeat testing of vision, eye movements, balance and cognition (which may include certain computer testing modules) before final clearance for contact sports.
Long Term Consequences
Many athletes and parents will ask the question “how many concussions is too many?” and again, the answer is not always straightforward. Most experts agree that any athlete that has 3 concussions in the same season should probably be held from further participation for the season. In younger athletes, physicians may be even more conservative and may decline to clear an athlete to return to the same season after a second concussion. However, for multi-sport athletes, year-round athletes, a frank discussion should occur between physician, athlete, and parent (for younger athletes) to decide the appropriate timing for return to full participation.
In recent years, there has been a lot of discussion about a condition known at Chronic Traumatic Encephalopathy or CTE. Many patients and parents what to know what is the risk of developing this condition. For now, we think that the risk of CTE may not necessarily related to an absolute number of concussions, but rather that the condition may be related to multiple so-called “sub-concussion blows”. These are multiple minor impacts sustained over an entire athletic career that may or may not cause acute concussion symptoms. A classic example is a boxer who is struck in the head multiple times during both practice and competition. Most of these impacts will not cause concussion symptoms, but over a lifetime the athlete may sustain thousands of impacts to the head. The cumulative effect of this trauma is unknown. Its not clear why some former athletes seem to have no lasting symptoms while others develop severe and life altering symptoms that include dementia, movement disorders, and severe mood changes. The good news is that there is a lot of research ongoing that we hope will help us understand the risk of long term consequences of head injuries.
Prevention
The best way to prevent concussion is to follow good training guidelines. This includes learning proper tackling and heading techniques. There is also good reason to think that certain activities such headers in soccer and tackling in football should be avoided in youth sports. Even in high school, college, and pro sports, many experts recommend limiting the number of contact practices each week. In addition, we should also encourage the use of properly fitting helmets for bicycles, scooters, skateboards, snowboards, skiing, etc. While there is no evidence that helmets actually reduce the frequency or severity of concussions- they can reduce the likelihood of more severe brain injuries.
Parting advice:
If you or your child has a head injury and you are concerned about a concussion- you should seek care from a physician who is very comfortable with the diagnosis and management of this complex condition.
:::
Korin Hudson, MD, FACEP, CAQ-SM works for MedStar Sports Medicine in Washington, DC.
Photo by Ben Hershey on Unsplash
